“A Model to Predict Survival in Patients With End-Stage Liver Disease”
Hepatology. 2001 Feb;33(2):464-70. [free full text]
—
Prior to the adoption of the Model for End-Stage Liver Disease (MELD) score for the allocation of liver transplants, the determination of medical urgency was dependent on the Child-Pugh score. The Child-Pugh score was limited by the inclusion of two subjective variables (severity of ascites and severity of encephalopathy), limited discriminatory ability, and a ceiling effect of laboratory abnormalities. Stakeholders sought an objective, continuous, generalizable index that more accurately and reliably represented disease severity. The MELD score had originally been developed in 2000 to estimate the survival of patients undergoing TIPS. The authors of this 2001 study hypothesized that the MELD score would accurately estimate short-term survival in a wide range of severities and etiologies of liver dysfunction and thus serve as a suitable replacement measure for the Child-Pugh score in the determination of medical urgency in transplant allocation.
This study reported a series of four retrospective validation cohorts for the use of MELD in prediction of mortality in advanced liver disease. The index MELD score was calculated for each patient. Death during follow-up was assessed by chart review.
MELD score = 3.8*ln([bilirubin])+11.2*ln(INR)+9.6*ln([Cr])+6.4*(etiology: 0 if cholestatic or alcoholic, 1 otherwise)
The primary study outcome was the concordance c-statistic between MELD score and 3-month survival. The c-statistic is equivalent to the area under receiver operating characteristic (AUROC). Per the authors, “a c-statistic between 0.8 and 0.9 indicates excellent diagnostic accuracy and a c-statistic greater than 0.7 is generally considered as a useful test.” (See page 455 for further explanation.) There was no reliable comparison statistic (e.g. c-statistic of MELD vs. that of Child-Pugh in all groups).
C-statistic for 3-month survival in the four cohorts ranged from 0.78 to 0.87 (no 95% CIs exceeded 1.0). There was minimal improvement in the c-statistics for 3-month survival with the individual addition of spontaneous bacterial peritonitis, variceal bleed, ascites, and encephalopathy to the MELD score (see Table 4, highest increase in c-statistic was 0.03). When the etiology of liver disease was excluded from the MELD score, there was minimal change in the c-statistics (see Table 5, all paired CIs overlap). C-statistics for 1-week mortality ranged from 0.80 to 0.95.
In conclusion, the MELD score is an excellent predictor of short-term mortality in patients with end-stage liver disease of diverse etiology and severity. Despite the retrospective nature of this study, this study represented a significant improvement upon the Child-Pugh score in determining medical urgency in patients who require liver transplant. In 2002, the United Network for Organ Sharing (UNOS) adopted a modified version of the MELD score for the prioritization of deceased-donor liver transplants in cirrhosis. Concurrent with the 2001 publication of this study, Wiesner et al. performed a prospective validation of the use of MELD in the allocation of liver transplantation. When published in 2003, it demonstrated that MELD score accurately predicted 3-month mortality among patients with chronic liver disease on the waitlist. The MELD score has also been validated in other conditions such as alcoholic hepatitis, hepatorenal syndrome, and acute liver failure (see UpToDate). Subsequent additions to the MELD score have come out over the years. In 2006, the MELD Exception Guidelines offered extra points for severe comorbidities (e.g HCC, hepatopulmonary syndrome). In January 2016, the MELDNa score was adopted and is now used for liver transplant prioritization.
References and Further Reading:
1. “A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts” (2000)
2. MDCalc “MELD Score”
3. Wiesner et al. “Model for end-stage liver disease (MELD) and allocation of donor livers” (2003)
4. Freeman Jr. et al. “MELD exception guidelines” (2006)
5. MELD @ 2 Minute Medicine
6. UpToDate “Model for End-stage Liver Disease (MELD)”
Summary by Duncan F. Moore, MD
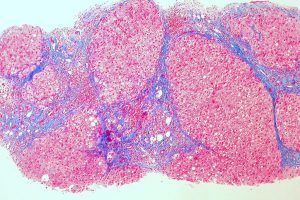
Image Credit: Ed Uthman, CC-BY-2.0, via WikiMedia Commons