“A Comparison of Rate Control and Rhythm Control in Patients with Atrial Fibrillation”
by the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) Investigators
N Engl J Med. 2002 Dec 5;347(23):1825-33. [free full text]
—
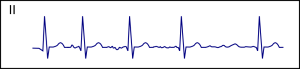
It seems like the majority of patients with atrial fibrillation that we encounter today in the inpatient setting are being treated with a rate-control strategy, as opposed to a rhythm-control strategy. There was a time when both approaches were considered acceptable, and perhaps rhythm control was even the preferred initial strategy. The AFFIRM trial was the landmark study to address this debate.
The trial randomized patients with atrial fibrillation (judged “likely to be recurrent”) aged 65 or older “or who had other risk factors for stroke or death” to either 1) a rhythm-control strategy with one or more drugs from a pre-specified list and/or cardioversion to achieve sinus rhythm or 2) a rate-control strategy with beta-blockers, CCBs, and/or digoxin to a target resting HR ≤ 80 and a six-minute walk test HR ≤ 110. The primary endpoint was death during follow-up. The major secondary endpoint was a composite of death, disabling stroke, disabling anoxic encephalopathy, major bleeding, and cardiac arrest.
4060 patients were randomized. Death occurred in 26.7% of rhythm-control patients versus 25.9% of rate-control patients (HR 1.15, 95% CI 0.99 – 1.34, p = 0.08). The composite secondary endpoint occurred in 32.0% of rhythm control-patients versus 32.7% of rate-control patients (p = 0.33). Rhythm-control strategy was associated with a higher risk of death among patients older than 65 and patients with CAD (see Figure 2). Additionally, rhythm-control patients were more likely to be hospitalized during follow-up (80.1% vs. 73.0%, p < 0.001) and to develop torsades de pointes (0.8% vs. 0.2%, p = 0.007).
This trial demonstrated that a rhythm-control strategy in atrial fibrillation offers no mortality benefit over a rate-control strategy. At the time of publication, the authors wrote that rate control was an “accepted, though often secondary alternative” to rhythm control. Their study clearly demonstrated that there was no significant mortality benefit to either strategy and that hospitalizations were greater in the rhythm-control group. In subgroup analysis that rhythm control led to higher mortality among the elderly and those with CAD. Notably, 37.5% of rhythm-control patients had crossed over to rate control strategy by 5 years of follow-up, whereas only 14.9% of rate-control patients had switched over to rhythm control.
But what does this study mean for our practice today? Generally speaking, rate control is preferred in most patients, particularly the elderly and patients with CHF, whereas rhythm control may be pursued in patients with persistent symptoms despite rate control, patients unable to achieve rate control on AV nodal agents alone, and patients younger than 65. Both the AHA/ACC (2014) and the European Society of Cardiology (2016) guidelines have extensive recommendations that detail specific patient scenarios.
Further Reading / References:
1. Cardiologytrials.org
2. AFFIRM @ Wiki Journal Club
3. AFFIRM @ 2 Minute Medicine
4. Visual abstract @ Visualmed
Summary by Duncan F. Moore, MD
Image Credit: Drj, CC BY-SA 3.0, via Wikimedia Commons